The Latest Addiction Statistics: U.S. Addiction Statistics in 2023
- Start Your Journey
- Mental Health & Co-Occurring Disorders
- Treatment Options for Adult ADHD at 12 South Recovery
- Substance Use & Mental Health by Age
- Key Takeaway
- Regional Differences
- Populations at Risk
- Alcohol: America’s Most Commonly Used Substance
- Opioids: A Crisis That’s Evolving, Not Ending
- Marijuana: Mainstream and Still Growing
- Stimulants: Cocaine, Meth, and ADHD Medication Misuse
- Treatment & Recovery: The Human Side of the Numbers
- Mental Health Shows Slight Improvement, But Gaps Remain
- Where and How People Get Treated
- When Mental Health and Addiction Overlap
- The Bright Side: Recovery Is Possible
- Why Don’t More People Seek Help
- Signs of Hope Are Emerging
- What Surprised Us in 2023
- Start Your Journey

Every year, the federal government runs a massive survey called the National Survey on Drug Use and Health (NSDUH). It’s designed to get a clearer picture of how many Americans are using substances, dealing with addiction, or facing mental health challenges. This report breaks down the latest numbers from the 2023 survey in a way that’s easy to understand because data should be useful, not overwhelming. Whether you’re a parent, a healthcare worker, someone in recovery, or just curious about what’s happening in your community, this information helps us all see the bigger picture.
We’ll walk through the key trends in substance use and mental health, point out which groups are most affected, and look at how things have shifted over the past few years. The more we understand the scope of these issues, the better equipped we are to respond with compassion, awareness, and action.
A Quick Look at the Data
The 2023 NSDUH included responses from tens of thousands of Americans aged 12 and up, across every state. It covers everything from alcohol and tobacco to marijuana, opioids, and mental health treatment. Because the survey’s methods changed in 2021, the most reliable comparisons are between 2021, 2022, and 2023. That’s where we’ll focus, on the trends that are shaping the current landscape and what they might mean going forward.
Substance Use in 2023: What the Numbers Say
Over Half of Americans Report Using Substances Regularly
Substance Use is more common than you might think. Nearly 6 in 10 Americans aged 12 or older used alcohol, nicotine, or drugs in the past month. That is around 167 million people! This includes legal substances like beer or cigarettes as well as illegal or misused ones. Substance use is woven into daily life for many, whether casually, socially, or in ways that may signal deeper struggles.
Alcohol Tops The List
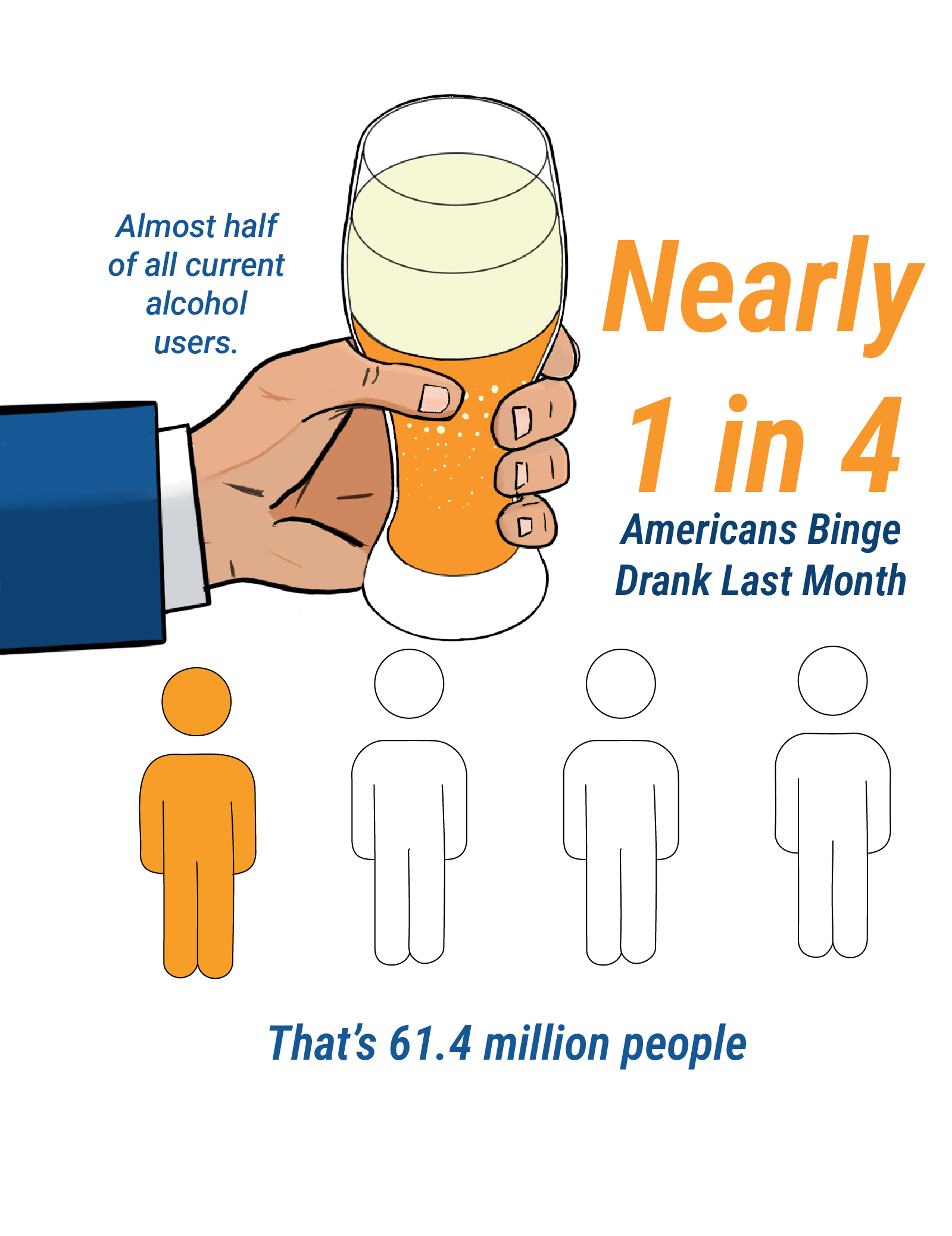
Alcohol remains the most widely used substance in the United States. In 2023, about 134.7 million people (roughly 47.5% of the population) reported drinking in the past month. And for many, it wasn’t just the occasional drink. Nearly half of current drinkers said they binge drank—having several drinks in a short span of time. That’s around 61.4 million people. Binge drinking is especially common among young adults. However, it’s not just a youth issue. About 1 in 4 American adults reported binge drinking recently.
Vaping Is Overtaking Cigarettes, Especially Among Teens
Tobacco use is changing. While about 49.9 million Americans (17.6%) used some kind of tobacco product in the past month, only 13.7% smoked traditional cigarettes—down from 16% in 2021. That’s a win for public health. But vaping is now the nicotine habit of choice, especially among teens. Of the youth who use nicotine, the vast majority are vaping rather than smoking. In 2023, 9.4% of Americans, 26.6 million people, vaped nicotine. (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health)
Marijuana Leads the Way in Widespread Illicit Drug Use
About 1 in 6 Americans (16.8%) used an illicit drug in the past month—roughly 47.7 million people. Looking over the whole year, nearly 1 in 4 (around 70 million people) used an illicit substance. Marijuana is by far the most common, used by 61.8 million people in 2023. That’s about 22% of the population. Compared to marijuana, use of other illicit drugs—like cocaine or opioids—is significantly lower, but still concerning. The growing acceptance and legalization of marijuana in many states is clearly reflected in these numbers. (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health).
Mental Health & Co-Occurring Disorders
At 12 South Recovery in Lake Forest, California, starting treatment for ADHD is a supportive and individualized process. Our team begins with a comprehensive assessment to understand each client’s unique challenges, symptoms, and goals. This thorough evaluation allows us to develop a personalized treatment plan tailored to address the specific ways ADHD impacts daily life. From the moment clients walk through our doors, they are met with compassion, expertise, and a safe environment designed to empower them on their journey toward better focus, productivity, and overall well-being.
Treatment Options for Adult ADHD at 12 South Recovery
Mental Health Struggles Are Widespread and Growing More Severe
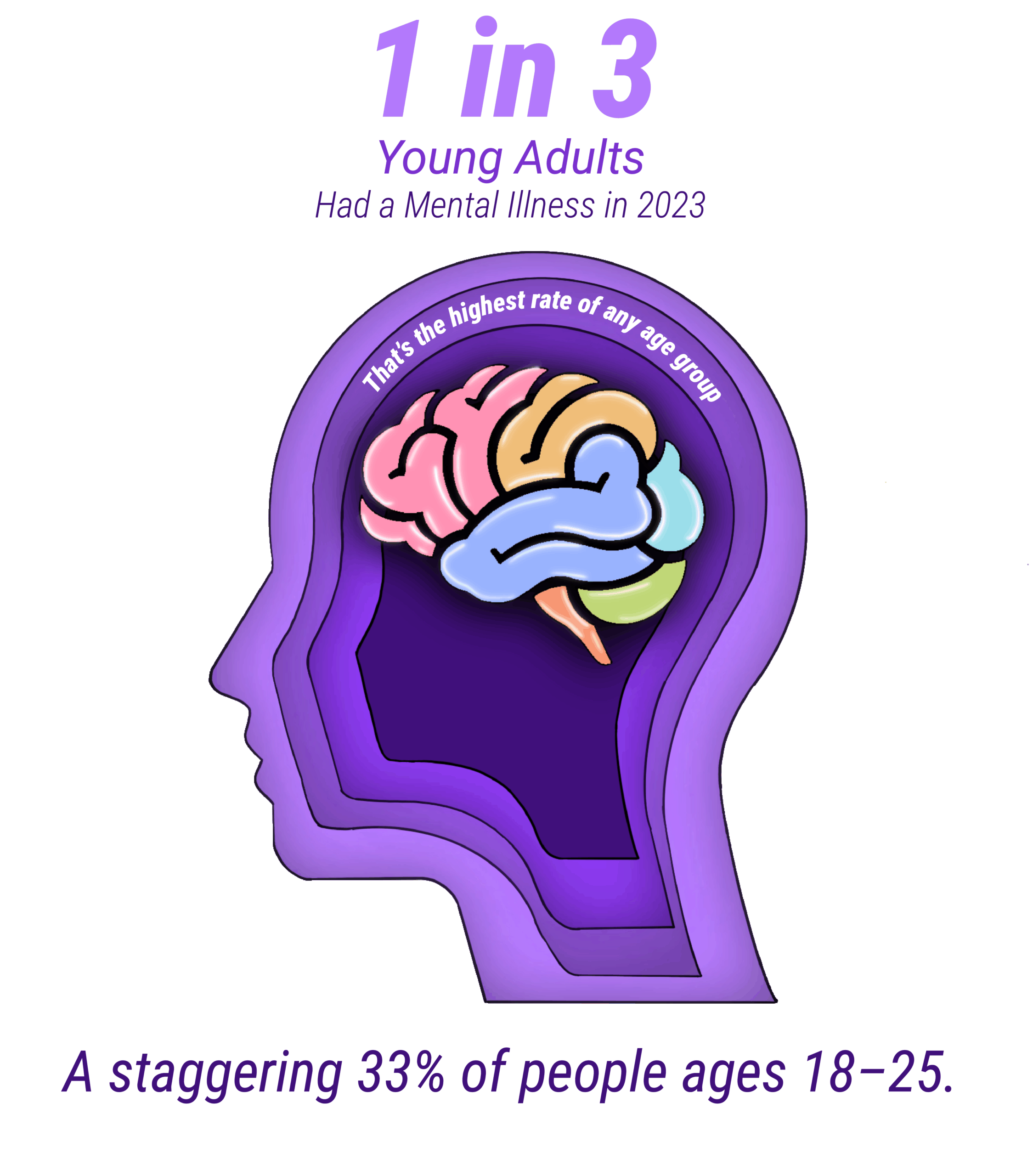
Substance use doesn’t happen in isolation. Often, it’s tied to deeper emotional or psychological struggles. In 2023, nearly 1 in 4 U.S. adults (22.8%, or about 58.7 million people) experienced some form of mental illness – anything from anxiety or depression to more severe conditions. About 1 in 20 adults (5.7%) faced a serious mental illness that made everyday life much harder.
Young adults are feeling it the most: nearly 1 in 3 people between 18 and 25 experienced mental health issues last year. And it’s not just adults. The mental health crisis is affecting teens too. In 2023, about 4.5 million adolescents (12–17 years old) had at least one major depressive episode. For many, it was serious enough to interfere with school, family, and friendships.
Substance Use and Mental Health Are Closely Connected
It’s not uncommon for someone struggling with mental health to also struggle with substance use – or vice versa. These are known as co-occurring disorders, and they’re more common than you might think. In 2023, about 48.5 million people had a substance use disorder (SUD), and a big portion of them also faced mental health challenges.
About 20.4 million adults had both a substance use disorder and a mental illness last year. Veterans, a group often at higher risk, showed similar overlap: roughly 1 in 20 had both conditions. The data is clear – if someone is dealing with anxiety, depression, or other mental health issues, they’re more likely to use substances.
In fact:
- 42.4% of adults with any mental illness used illicit drugs in the past year (compared to 21% of those without mental illness).
- Among people with serious mental illness, more than half (51.9%) used illicit drugs.
- Depressed teens were two and a half times more likely to use drugs than those without depression.
That’s why it’s so important to treat substance use and mental health together – one often feeds into the other.
Youth Suicidal Thoughts Are Alarmingly High
Perhaps the most heartbreaking numbers from the 2023 data involve teen suicidality. More than 3 million adolescents seriously considered suicide last year. Over 1.5 million made a plan, and 856,000 actually attempted it. That’s nearly 1 in 8 teens thinking about ending their life – a true crisis that affects families and communities everywhere.
Adults are struggling, too: 5% had serious thoughts of suicide, and 1.5 million adults attempted it. Many of these individuals are also battling substance use, which can make feelings of hopelessness even worse. These numbers are more than statistics – they reflect the emotional pain so many people are carrying.
Substance Use & Mental Health by Age
Age shapes a lot about how and why people use substances – and how likely they are to struggle with mental health.
Adolescents (12–17 years old):
Teen substance use is lower than among adults, but even small numbers are concerning at this age because the brain is still developing. In 2023:
- Around 2.2 million teens (8.5%) had a substance use disorder.
- 2.9 million (11.2%) used marijuana in the past year.
- Nearly 1 in 7 teens drank alcohol recently.
- 3.3 million teens (8.6%) binge drank, and 663,000 were heavy drinkers.
Teen smoking has dropped sharply, with only about 7.4% (1.9 million) using tobacco or vape products – and most of those vaped, rather than smoked. While that’s progress, nicotine addiction remains a concern, especially with flavored vaping products.
Mental health remains a big concern: 18% of teens had a depressive episode last year, and 12% seriously considered suicide. These struggles often go hand-in-hand with early substance use.
Young Adults (18–25 years old):
This age group leads the way in both substance use and mental health challenges – and often both at once.
- Over 36% used marijuana in the past year – the highest of any age group.
- Nearly 10 million (28.7%) were binge drinkers.
- About 1 in 4 young adults (27.1%) had a substance use disorder.
- 33.8% had any mental illness, and 10.3% had a serious mental illness.
When you combine those numbers, nearly half of all young adults were affected by addiction, mental illness, or both in 2023. That’s a staggering reality. These years are when many people begin facing emotional challenges or experiment with substances – and those patterns can stick. That makes this age group a critical target for education, early intervention, and mental health support.
Adults 26 and older:
As people get older, substance use tends to decline slightly – but because this age group is so large, it still contains the majority of people with addiction.
- 16.6% of adults 26+ (about 37 million) had a substance use disorder.
- 22.7% (50.6 million) binge drank in the past month.
- 20.8% (46.5 million) used marijuana.
Mental health issues vary within this group. Adults aged 26–49 had a 29.2% rate of mental illness, while those 50 and older had a lower (but still important) rate of 14.1%.
Older adults tend to use fewer illicit drugs but may misuse prescription medications – especially painkillers or sedatives. They’re also the least likely to get mental health care: only 18% of adults 50+ received treatment in 2022, compared to 25% of younger adults. That’s a missed opportunity to help a vulnerable group.
Key Takeaway
The earlier we can intervene, the better chance we have of preventing long-term struggles with addiction and mental health. This is especially important during the teen and young adult years. This isn’t just about statistics. It’s about understanding real people, real pain, and real opportunities to help. The data show us where the problems are most urgent, so we can focus our energy where it will matter most.
Regional Differences
Where you live in the U.S. can shape your experience with substance use and mental health. The National Survey on Drug Use and Health (NSDUH) highlights clear differences based on geography—whether that’s by state, region, or between rural and urban areas. Here are a few key takeaways:
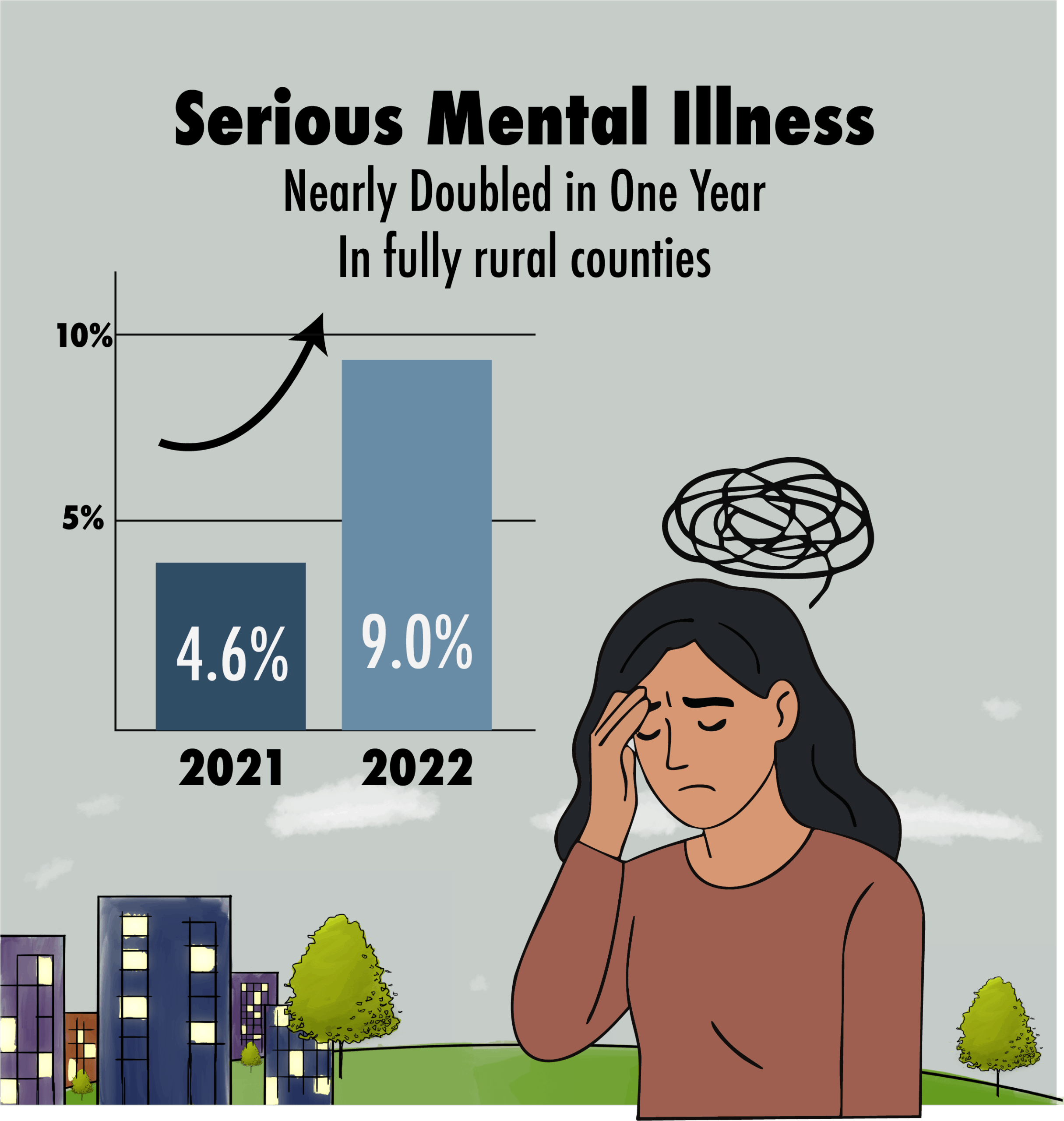
Urban vs. Rural:
Rural communities often face a tougher road when it comes to both substance use and mental health. For example, tobacco use among young adults is higher in rural areas. About 31.5% of 18–25-year-olds in non-metropolitan areas used tobacco in 2023, compared to 23.9% in large cities. That gap shows how nicotine addiction remains a bigger problem outside urban centers. Mental health challenges have also intensified in rural areas.(Substance Use and Misuse in Rural Areas Overview – Rural Health Information Hub). One analysis found that the rate of serious mental illness in completely rural counties nearly doubled from 4.6% in 2021 to 9.0% in 2022 (New Federal Data Offers Snapshot of America’s Substance Use …). Some of that increase may be linked to pandemic-related stress or changes in data collection methods. Still, it reveals a troubling trend—mental health needs are rising quickly in areas with limited access to care. Fewer local providers and less access to treatment services make it harder to get help. But there are bright spots. Tight-knit rural communities are well-positioned to benefit from telehealth, school and church-based outreach, and other creative solutions.
State and Regional Patterns:
Substance use doesn’t look the same in every part of the country. Western and Northeastern states tend to have higher rates of illicit drug use. Some Southern states report lower rates, though alcohol use remains fairly consistent nationwide. States like Alaska, Colorado, Oregon, D.C., Vermont, Maine, Massachusetts, and Rhode Island rank among those with the highest overall drug use. (2021-2022 National Survey on Drug Use and Health National Maps …). In some of these places, about 1 in 4 residents reported using illicit drugs in recent surveys—well above the national average. Meanwhile, some Southern and Midwestern states report lower drug use but may still struggle with alcohol or specific substances. These differences are often linked to local culture, such as more permissive attitudes toward marijuana. Economic stress or regional drug crises, like the opioid epidemic in Appalachia, also play a major role. Alcohol use also varies across regions. New England and parts of the Midwest report high rates of binge drinking. In contrast, some Southern states have lower alcohol consumption due to stricter laws or religious norms.
Opioids and Overdose Hotspots:
NSDUH focuses on drug use rather than overdose deaths, but other data show where the opioid crisis has hit hardest. States like West Virginia and Ohio have some of the highest overdose death rates in the country. NSDUH data reveal that misuse of prescription painkillers remains widespread—about 8.6 million Americans misused opioids in 2023. Rural areas have long been especially hard-hit by prescription opioid misuse, and more recently, by fentanyl. There isn’t a clear North/South or urban/rural divide in these patterns. Local prescribing habits and drug trafficking routes heavily influence regional substance use trends.In Summary:
Substance use and mental health challenges vary widely depending on where someone lives. Rural communities and certain high-use states are carrying heavier burdens, and that means solutions need to be local. What works in an urban setting—with easy access to clinics and specialists—may not be practical in a remote town. Recognizing these regional differences is critical if we want our prevention and treatment efforts to truly make an impact.
Populations at Risk
While addiction and mental illness affect people from all walks of life, some groups face steeper challenges. Understanding which populations are most at risk helps ensure that support and services reach those who need them most. Here’s a closer look at some of the key groups highlighted in the 2023 NSDUH data:
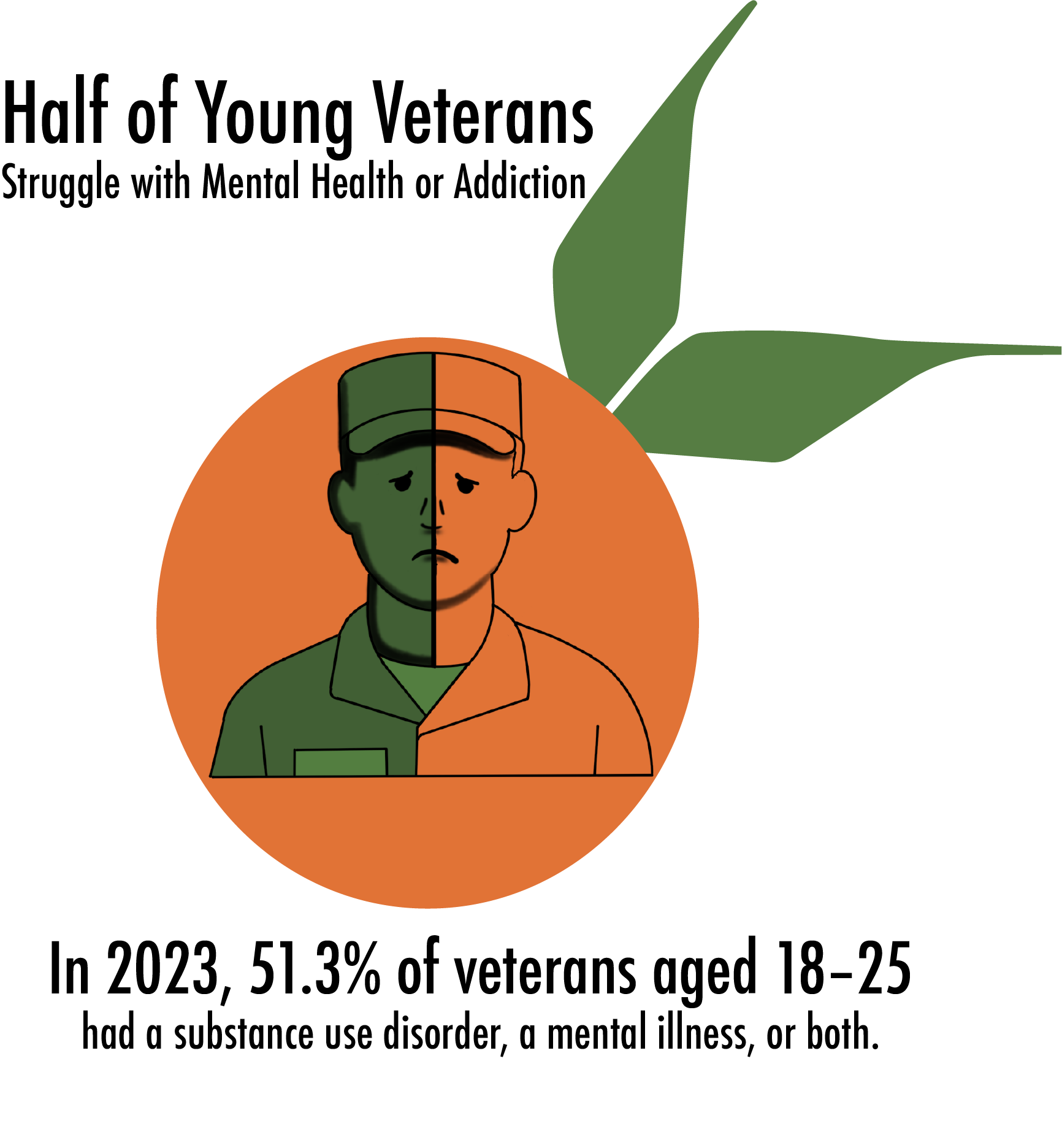
Veterans:
Military service can come with intense stress and trauma. This makes veterans especially vulnerable to mental health issues and substance use. Among young veterans (ages 18–25), about 51.3% experienced either a substance use disorder or a mental illness in the past year. Across all veterans, roughly 1 million are dealing with both simultaneously. The effects of PTSD, chronic pain, and the challenges of civilian life often overlap with substance misuse. The encouraging news: many veterans are finding their way to recovery. About 4 in 5 veterans who’ve had substance issues say they’re now “in recovery,” a rate higher than that of civilians. However, due to their elevated risk and high suicide rates, veterans remain a key priority for outreach, support, and specialized services.
Young People with Mental Health Struggles:
We mentioned this earlier, but it’s worth repeating. Teens and young adults battling mental health issues are at especially high risk for substance use and suicidal behavior. In 2023, around 856,000 adolescents had both a substance use disorder and major depression. These co-occurring issues often go untreated. Nearly 3 in 10 adolescents in this group received no mental health or substance use care at all. This is a serious gap in our healthcare system. Young adults (ages 18–25) are also deeply affected. Nearly half reported having either a substance use disorder or a mental illness. Reaching young people where they are—schools, campuses, workplaces, and online—is essential to turning the tide.
LGBTQ+ Youth:
Data consistently shows that lesbian, gay, bisexual, and transgender youth face significantly higher risks of mental health challenges. These include increased rates of depression, anxiety, and substance use. For instance, 37% of LGBTQ adolescents report experiencing depression—more than three times the rate among their heterosexual peers. (Recent Trends in Mental Health and Substance Use Concerns Among Adolescents | KFF). Many also report higher rates of drug use and vaping. The reasons are complex: bullying, trauma, family rejection, and lack of supportive healthcare all play a role. But there’s hope. Research shows that supportive environments dramatically reduce the risk of addiction and suicide among LGBTQ youth. This group stands out in the data, and efforts to support them can have life-saving results.
Racial and Ethnic Minorities:
Substance use prevalence can vary across racial and ethnic groups, but one major issue is treatment access. In 2022, treatment rates for adults with mental illness varied widely by race and ethnicity. Only 36% of Asian adults, 38% of Black adults, and 40% of Hispanic adults received care, compared to 56% of White adults. Similar disparities exist for substance use treatment. These gaps are shaped by systemic barriers: poverty, stigma, lack of access, and cultural mistrust of the healthcare system. Native American and Alaska Native communities face particularly high rates of substance use and overdose deaths, especially related to alcohol. These are urgent issues requiring culturally sensitive support, funding for tribal programs, and respect for traditional healing practices.
People with a History of Trauma:
This group isn’t defined by age, identity, or geography. However, trauma is a major underlying factor contributing to both addiction and mental illness. While the NSDUH doesn’t directly measure trauma, research shows a clear connection between early adversity—like abuse, neglect, or violence—and later substance use. Many of the at-risk groups above also experience high rates of trauma. Investing in trauma-informed care and early intervention could prevent countless future cases of addiction.
In Short:
Addiction and mental health challenges don’t affect everyone equally. Veterans, youth with mental illness, LGBTQ teens, communities of color, and people with trauma histories all show up in the data as needing more support. If you see yourself—or someone you care about—in one of these groups, know that you’re not alone, and that help is out there. Recognizing these risks is the first step toward building a system that meets people where they are and helps them heal.
Substance-Specific Trends: Alcohol, Opioids, Cannabis, and Stimulants
Let’s take a closer look at the most commonly used and misused substances in the United States. Some are increasing, some are declining, and others present serious public health challenges.
Alcohol: America’s Most Commonly Used Substance
Alcohol remains the most widely used – and misused – substance in the country. In 2023, about 134.7 million Americans, nearly half the population aged 12 and up, drank alcohol in the past month. Culturally and legally, alcohol is widely accepted, but that acceptance often masks the risks.
The bigger concern? Binge drinking. Defined as five or more drinks on one occasion for men, or four or more for women, binge drinking was reported by 61.4 million people – nearly half of all current drinkers. The numbers are especially high among:
- Young adults (18–25): 28.7% binge drank
- Adults 26+: 22.7%
- Teens (12–17): 3.9%, which equals about 1 million underage binge drinkers
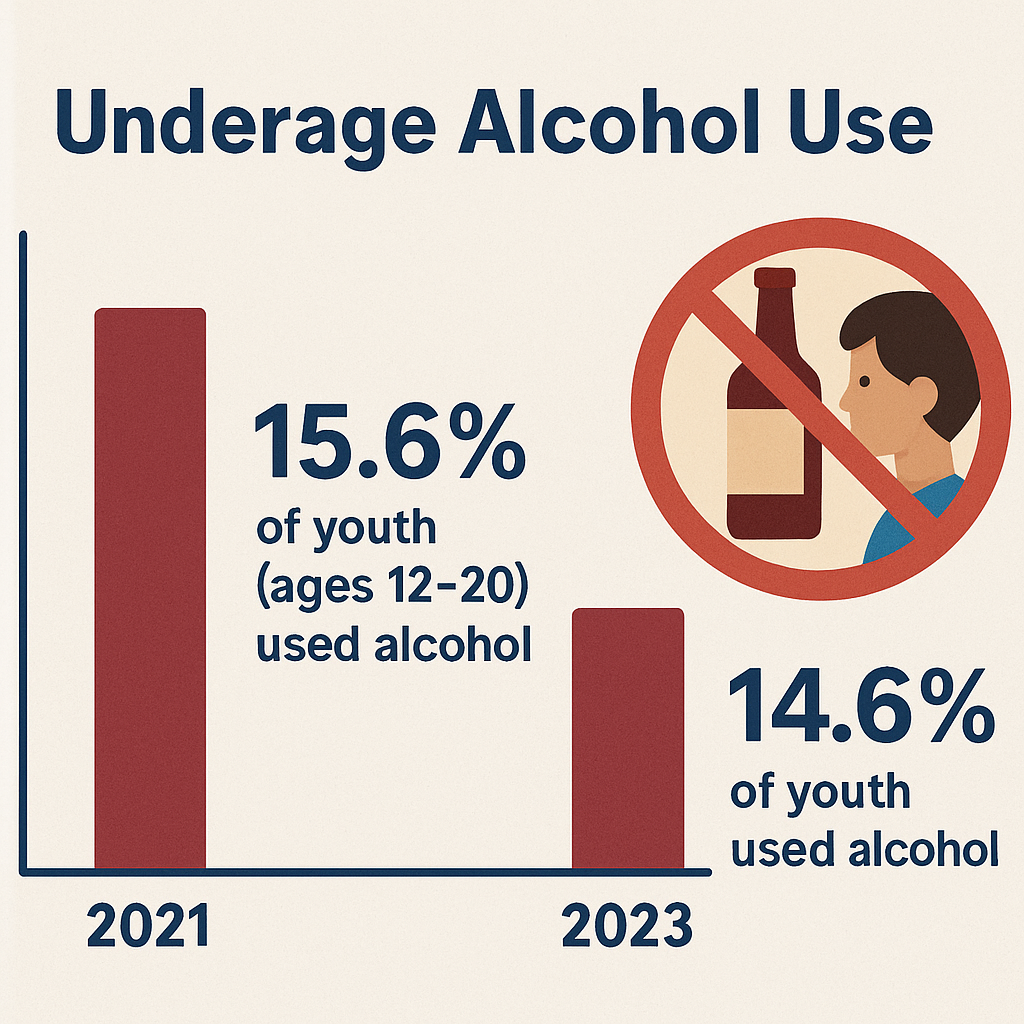
Although underage drinking has declined in recent years, it remains significant. In the past month, 5.6 million youth (14.6%) drank alcohol. Over 3 million of them reported binge drinking, and 663,000 were categorized as heavy alcohol users.
So when does drinking cross the line into an Alcohol Use Disorder (AUD)? According to the 2023 survey, 28.9 million people met the criteria for AUD. That’s about 1 in 9 Americans over age 12. Most cases are mild, but around 5–6 million had a severe alcohol disorder involving serious health and life consequences.
Key Takeaway: While youth drinking is on the decline, adult drinking habits haven’t improved much. Nearly half of drinkers binge, and AUD affects tens of millions. Continuing to educate young people and shift the binge drinking culture among young adults remains critical.
Opioids: A Crisis That’s Evolving, Not Ending
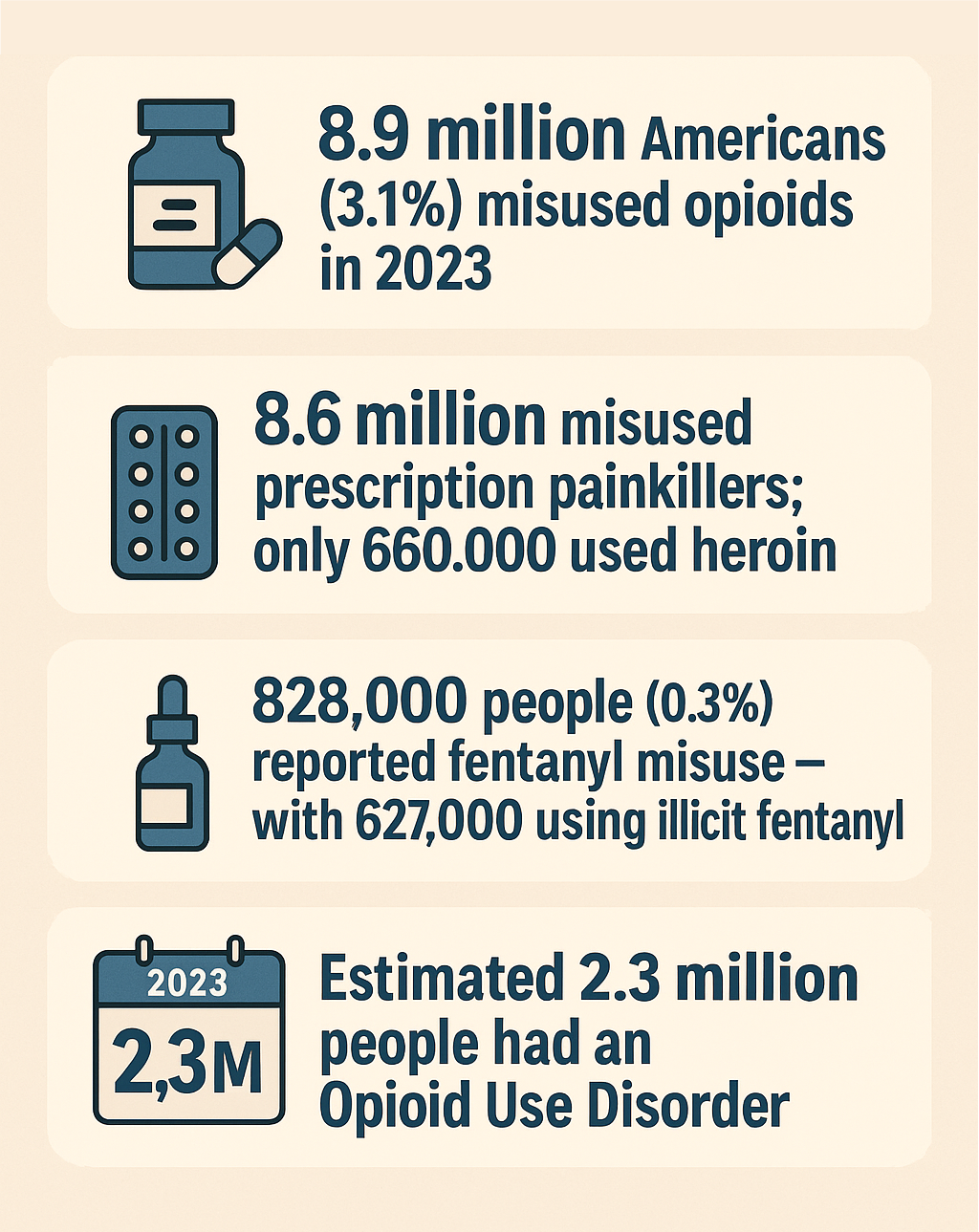
The opioid epidemic continues to evolve. In 2023, 8.9 million Americans (3.1%) misused opioids – either through non-medical use of prescription painkillers or using heroin. Most of that misuse (8.6 million people) involved pain medications like oxycodone and hydrocodone. Heroin use, by comparison, was much lower at 660,000 people, and only 336,000 used both.
The real game-changer? Fentanyl. This synthetic opioid is incredibly potent and increasingly common – often mixed into other drugs without the user’s knowledge. The 2023 survey reported:
- 828,000 people used fentanyl (either prescribed or illicit)
- 627,000 used illicitly manufactured fentanyl
These numbers may seem small, but the reality is far worse. Many users don’t even know they’re taking fentanyl, which is why overdose deaths continue to rise.
Though heroin use is declining, prescription misuse remains stubbornly high. Around 2.3 million people are estimated to have Opioid Use Disorder (OUD). However, only a small fraction receive treatment with medications like buprenorphine or methadone.
Key Takeaway: Prescription opioids are still driving the crisis. And with fentanyl in the mix, even “steady” user numbers can mean rising fatalities. Expanding access to treatment and overdose prevention tools like naloxone is essential.
Marijuana: Mainstream and Still Growing
Marijuana has become the most widely used illicit drug in the U.S., thanks in part to expanding legalization. In 2023, 61.8 million people (21.8%) reported using marijuana in the past year – that’s more than 1 in 5 Americans.
- Young adults (18–25): 36.5% used marijuana – making it practically the norm in this age group
- Adults 26+: 20.8%
- Teens (12–17): 11.2% (about 2.9 million youth), up from previous years
([PDF] Highlights for the 2022 National Survey on Drug Use and Health)
While annual use tells part of the story, daily or near-daily use is on the rise too, especially among college-aged users. Frequent use is more likely to lead to Cannabis Use Disorder, which affected 19.2 million people in 2023. That’s nearly 1 in 3 past-year users. Of those, about 3.5 million had a severe marijuana addiction.
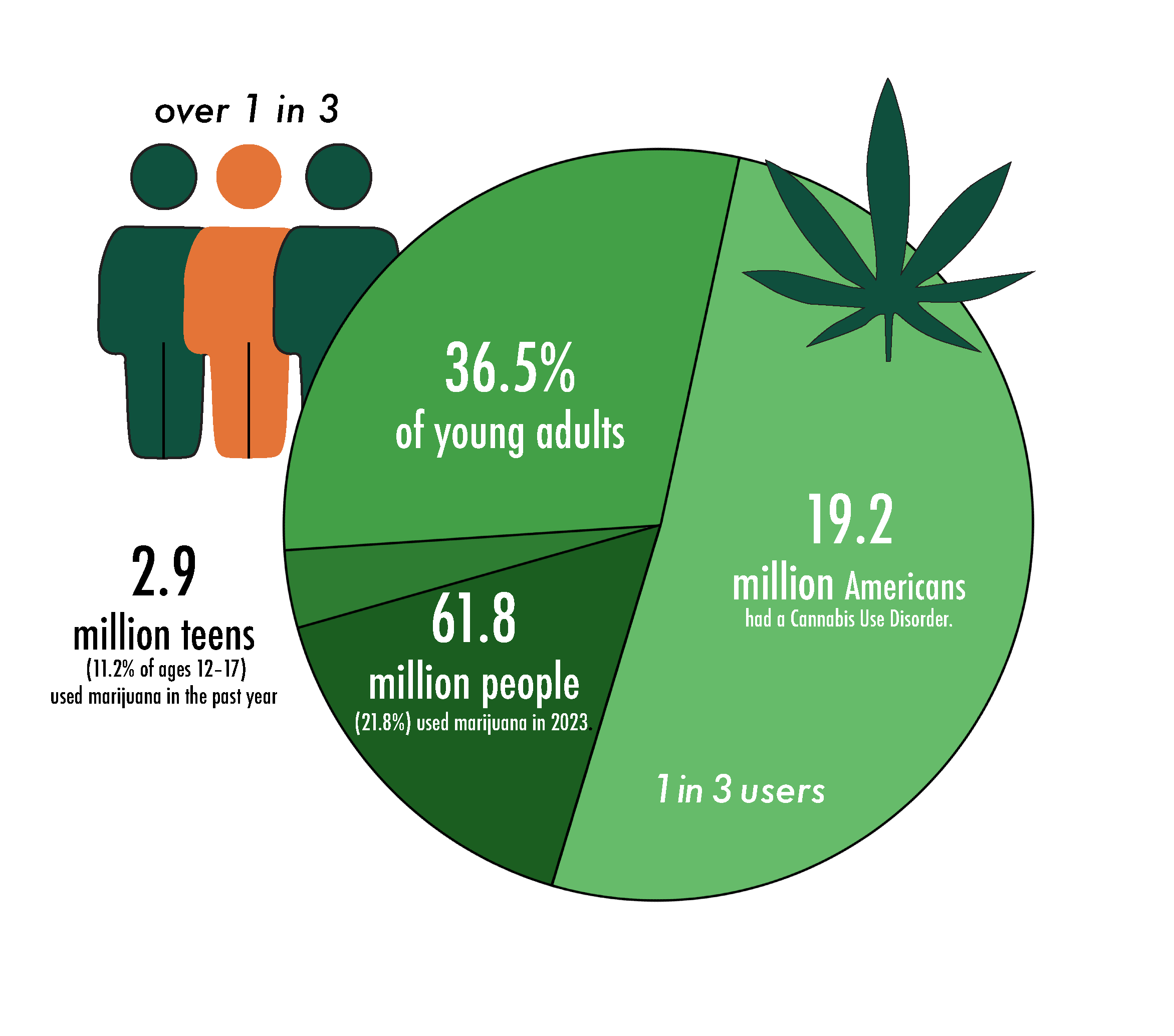
There’s a common belief that marijuana isn’t addictive. But the data shows that for millions, it can lead to real impairment – from trouble at work or school to mental health impacts.Key Takeaway: Marijuana use surged post-pandemic and has stayed high. With growing normalization, it’s important not to ignore the potential risks – especially for youth and frequent users.
Stimulants: Cocaine, Meth, and ADHD Medication Misuse
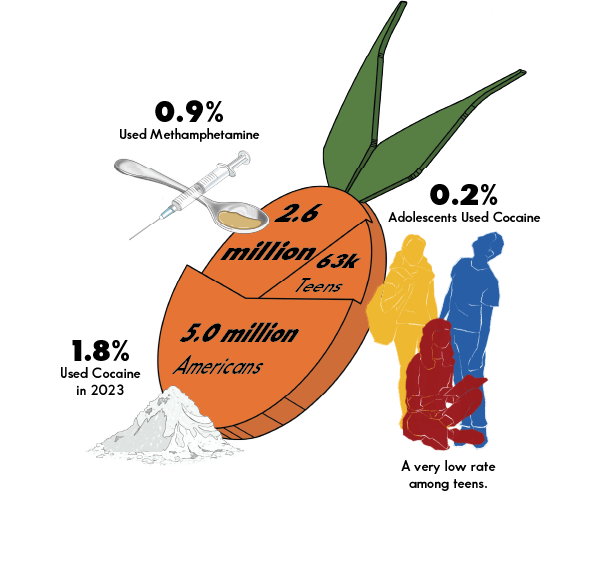
Stimulant misuse doesn’t attract as much attention as opioids. However, it remains a serious concern—especially with the growing presence of fentanyl in the drug supply.
Cocaine:
- 5.0 million people (1.8%) used cocaine in 2023
- Use is highest among young adults (3.1%), though most users are adults over 26
- Only 63,000 teens (0.2%) reported using it – a low, but still worrying figure
- Cocaine use hasn’t grown significantly, but fentanyl contamination is making it more deadly
Methamphetamine:
- 2.6 million people (0.9%) used meth in 2023
- More common in rural and western states
- Meth use has increased since the early 2010s – partially due to people switching from opioids
Prescription Stimulants (like Adderall):
Often used non-medically by students or professionals, prescription stimulant misuse is part of the broader stimulant category. In 2023, about 3.4% of Americans misused some form of stimulant. This includes substances like cocaine, methamphetamine, or ADHD medications.
Key Takeaway: Stimulant misuse isn’t as common as alcohol or marijuana use. However, it can be just as dangerous, especially with the increasing presence of fentanyl. Misuse of prescription meds like Adderall also deserves more attention, especially on campuses and in high-pressure work environments.
Tobacco and Nicotine
Tobacco & Nicotine remain among the most addictive substances in the U.S., though often left out of addiction conversations. Cigarette use is declining, but nicotine vaping is on the rise – especially among youth.
Cigarettes
13.7% of Americans smoked cigarettes in 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) which is down from 16.0% in 2021 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). That’s a big win for public health – smoking rates are now about one-third of what they were in the 1960s.Only 1.2 million underage youth currently smoke but smoking still kills more Americans than any other substance – over 400,000 deaths a year. Rural and lower-income populations still show higher smoking rates.
– Young adults in rural areas: 31.5% smoke vs. 23.9% in metro areas (Substance Use and Misuse in Rural Areas Overview – Rural Health Information Hub).
Many current smokers are long-term users facing tough nicotine addiction.
Vaping (E-cigarettes)
9.4% of Americans vaped nicotine in the past month (2023) which is up from 8.3% in 2022 (SAMHSA Releases 2023 NSDUH Substance Use Estimates).
Roughly 26.6 million people vape nationwide and 5.9 million tried vaping for the first time in 2023 – more than any other substance. Among youth who use nicotine, 75% use e-cigarettes only. Vaping is now the most common entry point for substance use among teens and young adults.
Attractive factors: fruity flavors, easy to hide, seen as “safer” than smoking but nicotine is still highly addictive – regardless of how it’s delivered.Early research shows vaping may affect brain development and increase addiction risk.
Public health debate: Can vaping help adult smokers quit without hooking a new generation?
Other tobacco products (cigars, chew, hookah, etc.)
17.6% of Americans used any tobacco product in 2023
But the majority of nicotine use still comes from cigarettes and vaping
Key Takeaway: Smoking is down, but vaping is way up – especially among teens. Nicotine addiction hasn’t gone away, it’s just shifted form. As access and appeal continue to grow, especially for youth, education is critical to prevent lifelong addiction.
Treatment & Recovery: The Human Side of the Numbers
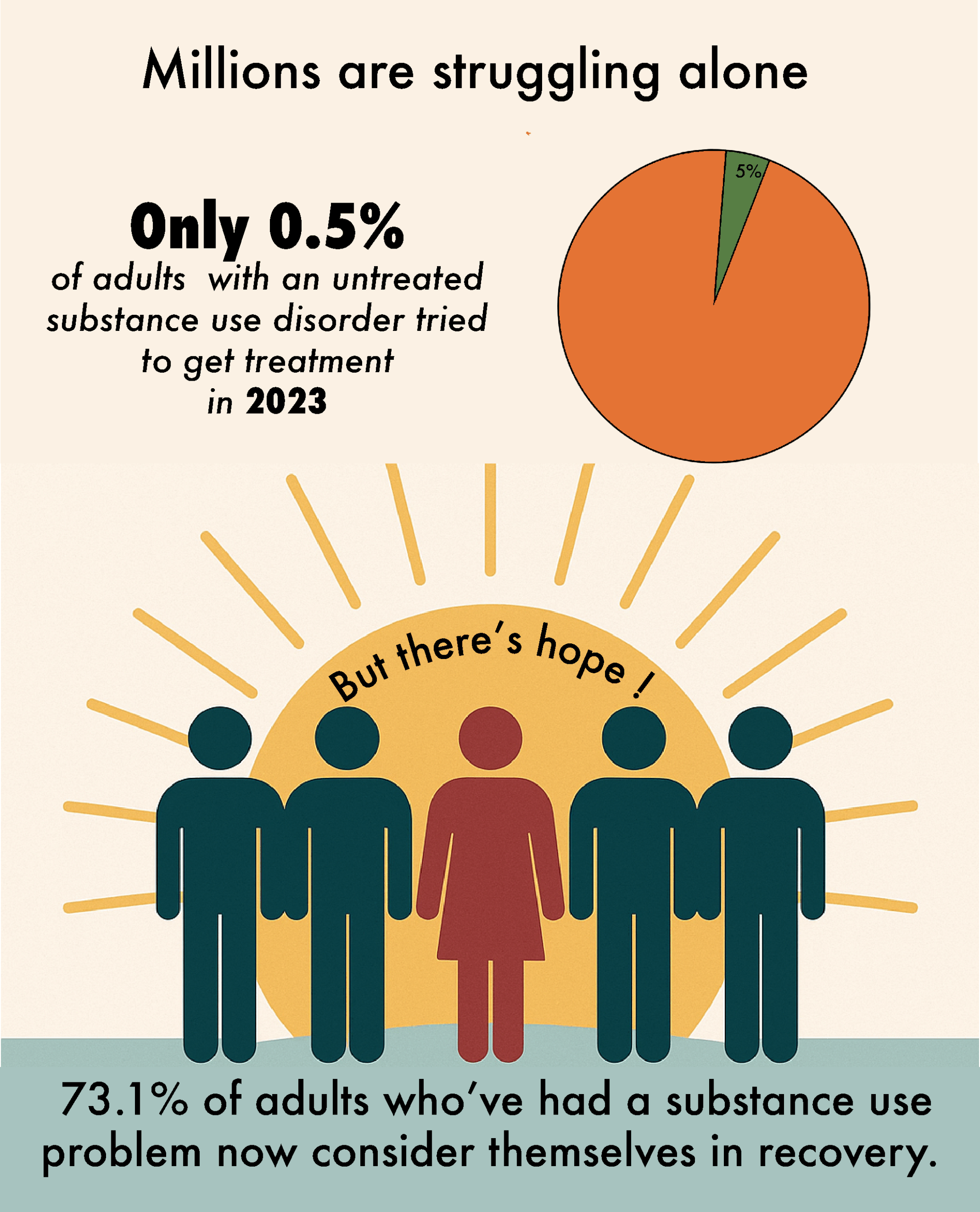
When we talk about addiction or mental health, numbers only tell part of the story. Yes, it’s important to understand how many people are struggling. But what truly matters is how many are getting help and finding a path toward recovery. The latest NSDUH data paints a picture that’s both sobering and hopeful.
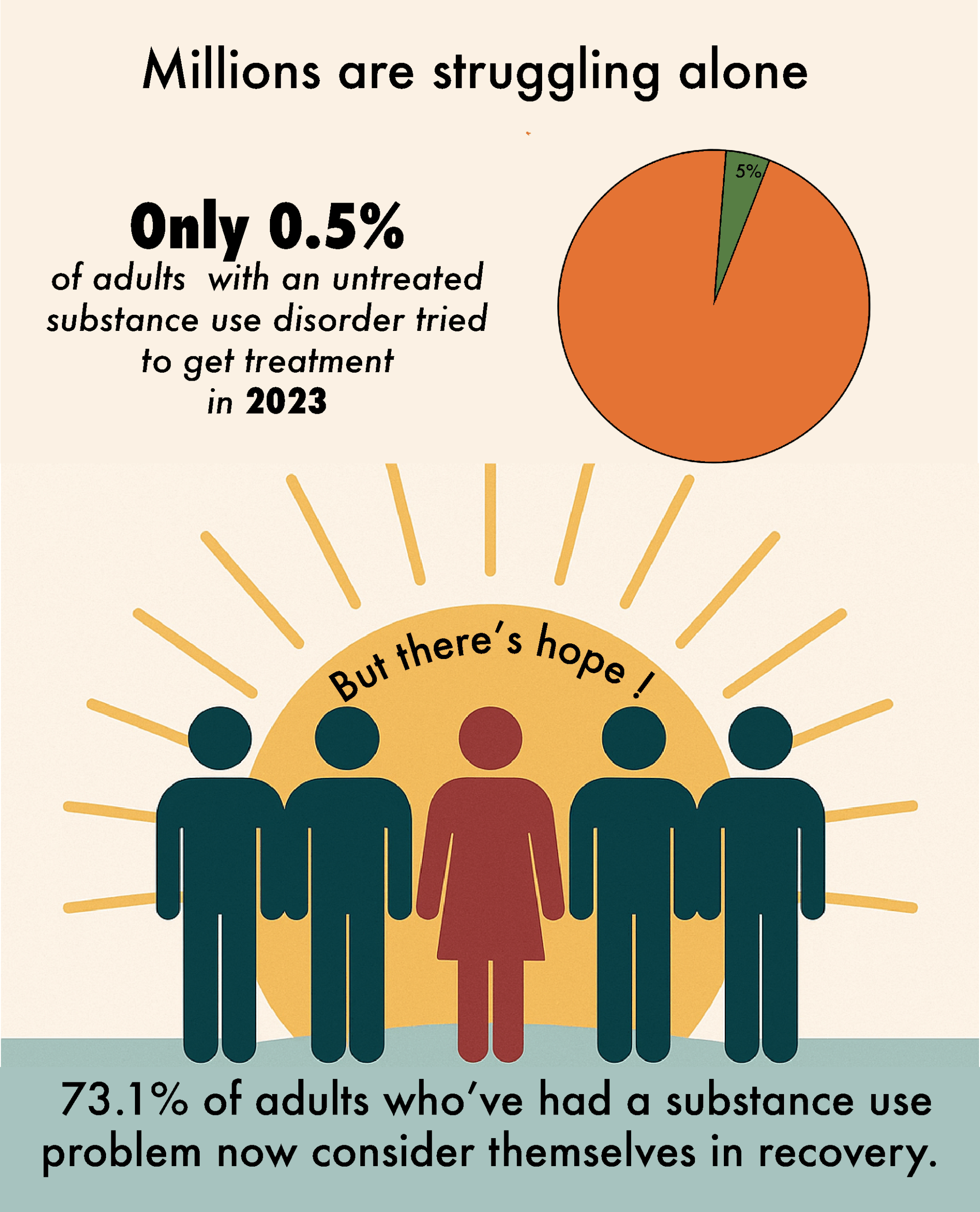
Most People Still Aren’t Getting the Help They Need
Let’s start with the hard truth: most people dealing with addiction or mental health issues aren’t in treatment. In 2023, nearly 49 million people in the U.S. had a substance use disorder (SUD). However, only about 1 in 4 of them received any kind of formal treatment. That means roughly 76%—tens of millions—didn’t get professional help.
The biggest reason? Most didn’t even think they needed it. In 2023, nearly 49 million people in the U.S. had a substance use disorder (SUD), but only about 1 in 4 received formal treatment. Of the nearly 40 million adults with an untreated SUD, over 94% didn’t seek help because they either didn’t believe they had a problem or didn’t want assistance. Only a tiny fraction, less than 1%, actively tried to get treatment but couldn’t.
It’s a similar story with teens. About 1.8 million adolescents had an SUD but didn’t get treatment. Almost all of them—96.6%—either didn’t think they needed help or didn’t try to find it. Just 9,000 teens (yes, nine thousand) actually went looking for treatment.
These numbers are staggering. They show that addiction isn’t just about access to rehab—it’s about recognition. If people don’t think they have a problem, they’re not going to ask for help. Stigma, denial, or the belief that they can “handle it on their own” are massive barriers.
Mental Health Shows Slight Improvement, But Gaps Remain
The treatment gap for mental health is smaller, but still big. About 59 million adults got some form of mental health treatment in 2023—counseling, medication, or both. Among adults with any mental illness, just over half (53.9%) received care. That’s progress, but it still means millions are going without.
For those with serious mental illness, things like schizophrenia or major depression, treatment rates were higher (71.1%), but nearly 1 in 3 still went untreated.
Teens with depression saw similar trends. About 60% got help, which is actually better than the rate for adults. But that still leaves 40%—hundreds of thousands of young people—dealing with depression on their own.
Why don’t people get care? For many, it’s cost, not knowing where to go, or fear that it won’t actually help. And again, some just don’t believe their problem is “serious enough.”
Where and How People Get Treated
The 2023 survey counts treatment in many settings—like inpatient, outpatient, telehealth ([PDF] Results from the 2023 National Survey on Drug Use and Health), and even jails. It doesn’t include things like peer support groups or emergency room visits unless they lead to formal treatment.
One big shift is the rise of telehealth. After COVID, virtual therapy and addiction treatment became much more common. While the report doesn’t break those numbers out, they’re included in the totals. For many people, being able to get help from home—on a phone or computer—makes treatment far more accessible.
When Mental Health and Addiction Overlap
Lots of people struggle with both mental health issues and substance use. Among teens with both depression and a substance use disorder (SUD), 71% received some form of treatment. However, most were treated only for their mental health, not their substance use. The same goes for adults: of those with both conditions, 62% got treatment (usually just for mental health), and nearly 38% got nothing.
This points to a problem in how our system works—we tend to treat one issue while ignoring the other. True recovery often means treating both at the same time.
The Bright Side: Recovery Is Possible
Here’s the encouraging part. Of the 30.5 million adults who said they’ve had a substance problem in their lifetime, more than 73% consider themselves “in recovery” now. That’s over 22 million people who’ve found a path forward. For mental health, the pattern is similar. About 64 million people reported having experienced a mental health issue at some point, and two-thirds say they are now in recovery or doing better.
That’s powerful. It shows that recovery isn’t just possible—it’s happening every day, for millions of people.
Veterans, in particular, showed even higher recovery rates. Nearly 80% of those with substance issues and 68% with mental health conditions say they’re in recovery. This might reflect the strong support systems available in veteran communities.
Why Don’t More People Seek Help
The data is clear: the biggest barrier isn’t always lack of access—it’s that people don’t think they need help. More than 9 out of 10 people with addiction never seek treatment. Many don’t even recognize the severity of their situation until something drastic happens.
Stigma also plays a huge role. People fear being judged or punished for admitting they have a problem. And then there are practical issues—like affordability, lack of insurance, or not having nearby programs, especially in rural areas.
For mental health, some people think they should just “tough it out” or that they’re not sick enough to need help.
Signs of Hope Are Emerging
Some promising trends are emerging. Medication-assisted treatment (MAT) for opioid addiction is becoming more common. More people are open to therapy, especially post-COVID. And the rise of telehealth is removing barriers for many who couldn’t access treatment before.
If these trends continue, we might start to see more people getting the help they need—and sooner.
What Surprised Us in 2023
Some of the trends from this year’s survey were expected. But a few results jumped out—either because they bucked recent patterns or raised new red flags. Here’s a look at what stood out:
Vaping Is the New Gateway Drug
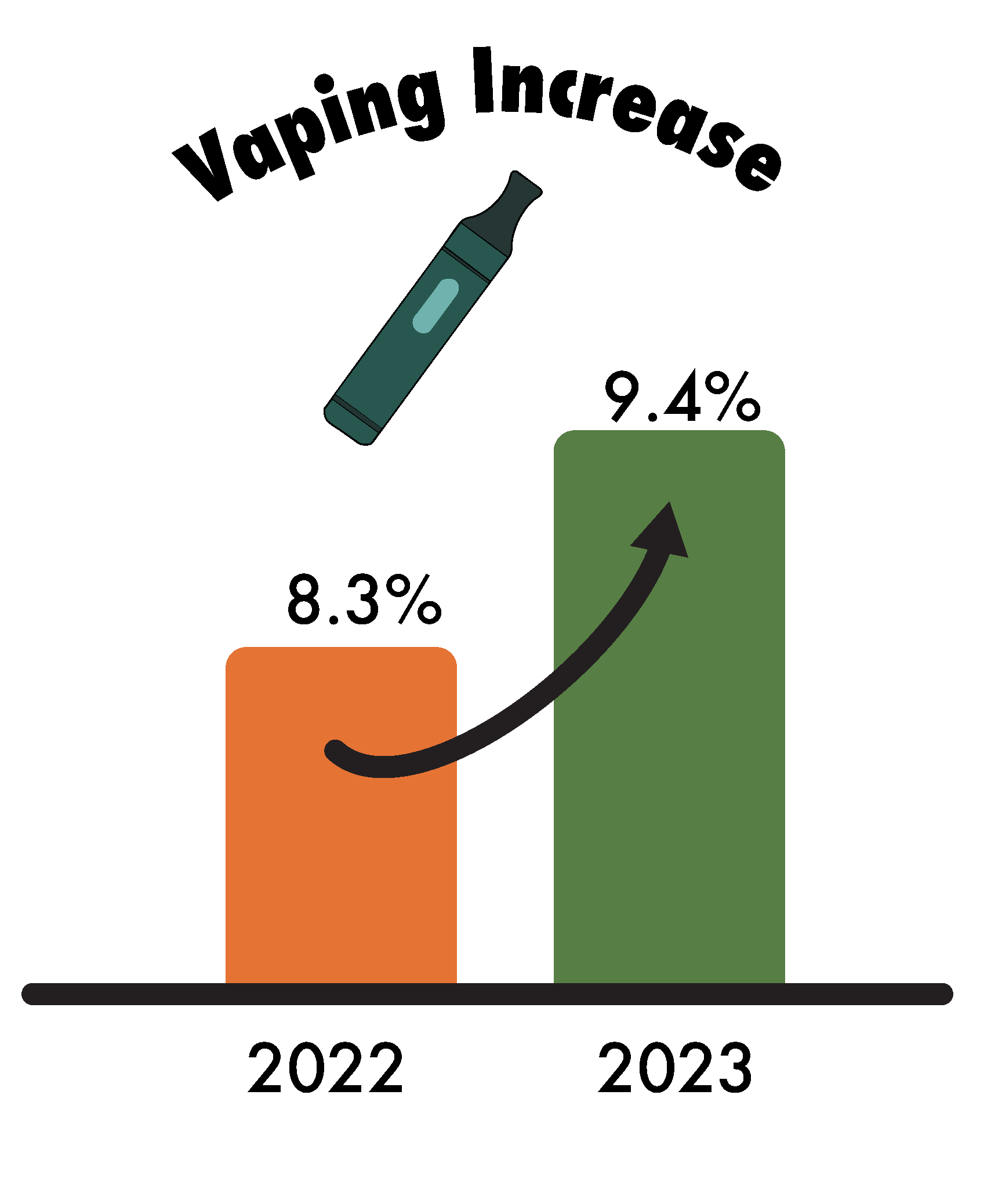
One of the most eye-catching changes? Nicotine vaping is exploding—especially among new users. The percentage of Americans who vape jumped from 8.3% in 2022 to 9.4% in 2023 (SAMHSA Releases 2023 NSDUH Substance Use Estimates). That may not sound massive, but it means millions more people picked up vaping last year.
Even more striking: more people tried vaping (5.9 million) than started using alcohol or marijuana. That officially makes vaping the #1 “gateway” substance for new users in 2023.
What’s driving this? Flavored e-cigarettes, slick marketing, and a lingering myth that vaping is safer than smoking. And while smoking rates are down, vaping has picked up the slack. In 2017, only about 4–5% of people vaped. Now it’s nearly 10% and climbing. Public health experts are sounding the alarm. We may be winning the cigarette war, but losing the vaping battle.
A Tiny Glimmer of Hope for Teen Mental Health
After years of worsening numbers, teen mental health may have finally hit a turning point. The percentage of adolescents with major depression dropped slightly—from 19.5% in 2022 to 18.1% in 2023. (Recent Trends in Mental Health and Substance Use Concerns Among Adolescents | KFF)
Yes, that’s still nearly 1 in 5 teens—but it’s the first sign of improvement in a long time. And in a year when many expected things to stay flat or get worse, even a small drop feels meaningful. Reopened schools, more social interaction, and greater focus on mental health resources could be playing a role.
Too early to declare victory? Definitely. But for now, it’s a rare bit of good news.
Heroin Use Is Down But Fentanyl Is Hiding in Plain Sight
Here’s a head-scratcher: heroin use is at an all-time low (just 0.2% of the population). That might sound like a win because heroin used to be the poster child of the opioid epidemic.
But hold the celebration.
What’s actually happening is that many people who used heroin have switched to something even more dangerous: fentanyl. And here’s the kicker, most people don’t even know they’re using it. Fentanyl is showing up in counterfeit pills and laced into street drugs, often without users realizing it.
Only 0.3% reported using fentanyl, yet it’s behind record overdose deaths. That disconnect tells us the data isn’t capturing the full picture. Heroin is down, but the risk? Sky high.
Almost Half of Young Adults Are Struggling
It’s no secret that young adults (ages 18–25) are facing a mental health and addiction crisis—but the numbers still shocked us: 46.9% of them had either a mental illness or substance use disorder in 2023. That’s nearly half.
The stat actually dipped slightly from 48.8% the year before, but still—it paints a stark picture. For college campuses, workplaces, and families, this confirms what many already feel: supporting this age group is now a critical priority, not just a nice-to-have.
Most People with Addiction Still Aren’t Getting Help
This one’s as frustrating as it is familiar: over 94% of people with a substance use disorder didn’t get any treatment in 2023—and most didn’t even try to.
In fact, the percentage of adults with addiction who sought help dropped slightly—from 0.8% in 2022 to just 0.5% in 2023. That means only 1 in 200 people with addiction made any attempt to get treatment last year.
Despite all the progress in telehealth, awareness campaigns, and access to care, this stat hasn’t really budged. The message is clear: treatment can’t help if people don’t believe they need it.
Teen Smoking Rates Drop Significantly, But with a Catch
One major win: underage cigarette smoking dropped like a rock—from 4.5 million teen smokers in 2021 to just 1.2 million in 2023. (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health).
That’s an enormous decline, and it shows that decades of anti-smoking efforts have paid off. Today’s teens just aren’t interested in lighting up traditional cigarettes.
But here’s the catch: many of them are vaping instead. So while we’re seeing fewer smokers, we’re not necessarily seeing fewer nicotine users. It’s a public health victory with an asterisk.
Smaller Shifts Worth Mentioning
Overall drug use is up, then leveled off: Illicit drug use climbed from 22.2% in 2021 to 24.9% in 2022, and stayed there in 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). Some of that increase may be due to wider marijuana legalization. Still, it suggests we’ve hit a new baseline rather than continuing to climb.
Meth use is creeping back: It’s a slow rise, but methamphetamine use grew from around 0.7% to 0.9%. Not explosive—but not going away either. Experts are keeping a close eye on this one.
More people now say they’re “in recovery”: That’s a pleasant surprise. More former users are embracing the recovery identity. Public campaigns and shifting attitudes about addiction are helping to reduce stigma, and it’s showing up in the data.
In short, the 2023 numbers don’t bring dramatic swings, but they do reveal important shifts. Vaping is accelerating. Fentanyl is distorting what we think we know about opioid use. Teen smoking may be ending, but youth nicotine use isn’t. And the treatment gap remains a stubborn wall.
There’s progress, but also new pitfalls. Staying informed and responsive is more important than ever.
Looking at the Trends: What’s Changed from 2021 to 2023
While experts caution against drawing big conclusions from just three years of data—especially since the way the survey was done changed in 2021—we can still get a pretty good sense of where things are headed when it comes to substance use and mental health in the U.S. Here’s a snapshot of what we’ve seen between 2021 and 2023 (2023 National Survey on Drug Use and Health (NSDUH) Releases | CBHSQ Data) (2023 National Survey on Drug Use and Health (NSDUH) Releases | CBHSQ Data):
Illicit Drug Use Spiked, Then Leveled Off
Illicit drug use jumped noticeably from 2021 to 2022—rising from about 22% to 25% (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) of the population. But from 2022 to 2023, it barely budged, staying right around 24.9%. That suggests the spike may have been partly due to how the survey changed or the lingering effects of the pandemic. Now, we seem to be settling into a “new normal.”Marijuana use followed a similar pattern. It rose from 19% in 2021 to about 22% in 2022, and then held steady through 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). In short, we saw a surge—and now, things have leveled off. People who were open to using cannabis may have already made the switch, and new use isn’t accelerating like it was.
Nicotine: Smoking Down, Vaping Up
Here’s some good news: cigarette smoking among adults dropped from 16.0% in 2021 to 13.7% in 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). That’s a solid decline. But there’s a flip side—vaping is on the rise. Nicotine vaping increased to 9.4% in 2023, with the most noticeable bump occurring between 2022 and 2023.
Among young people, this shift is even more dramatic. In 2021, around 16% of youth smoked cigarettes while about 11% vaped. Fast forward to 2023, and only 5% were smoking—but nearly 13% were vaping (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health) (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). The bottom line? Traditional smoking continues to decline, but e-cigarettes are filling that void.
Teen Substance Use: Mostly Stable, With a Few Tweaks
For adolescents, substance use hasn’t changed much over the past few years:
- Alcohol use (ages 12–20) dipped slightly from 15.6% in 2021 to 14.6% in 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). Binge drinking stayed relatively flat—around 8.6% in 2021 and 2023, with a small dip in 2022.
- Marijuana use among teens rose a bit in 2022 (from 17.9% to 19.2%) but dropped to 18.4% in 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health). These changes aren’t statistically significant, meaning the trend is essentially flat.
- Other illicit drug use—like misuse of prescription meds or harder substances—remains low (under 5%) and steady.
So while teen cannabis use remains historically high, it doesn’t appear to be climbing further post-legalization—at least for now.
Substance Use Disorders (SUDs): Holding Steady
Roughly 17% of adults had a substance use disorder in each of the past three years—46.3 million people in 2021, 48.7 million in 2022, and 48.5 million in 2023. That’s not a dramatic shift, which is noteworthy considering the stress and isolation brought on by the pandemic.
Alcohol use disorders may have ticked down slightly (from 29.5 million to 28.9 million), while drug use disorders stayed about the same (27.2 million both years). Overall, it looks like increased casual use (especially marijuana) didn’t lead to a surge in addiction.
Mental Health: A Surge, Then a Possible Plateau
Mental health concerns rose during the pandemic—and while they remain high, there’s some evidence they’re no longer climbing.
- Any Mental Illness (AMI) among adults went from about 22% in 2021 to 22.8% in 2023.
- Serious Mental Illness (SMI) peaked at 6% in 2022 and slightly dipped to 5.7% in 2023 (2023 Companion Infographic Report: Results from the 2021, 2022, and 2023 National Surveys on Drug Use and Health).
- Among teens, the rate of major depressive episodes hit a high of 19.5% in 2022 but dropped to 18.1% in 2023.
That small decline in youth depression may be a sign the worst has passed—but it’s too soon to be sure. Even if the rates are leveling off, today’s mental health challenges are still far greater than what we saw a decade ago.
Treatment & Recovery: Progress Is Slow, But There’s Hope
Traditionally, only about 1 in 10 people with a substance use issue received treatment. The definition of “treatment” changed in 2022, so we can’t make long-term comparisons, but here’s what we do know:
The percentage of people who say they’re in recovery rose slightly—from 71% in 2022 to 73% in 2023. That’s encouraging and points to a growing recovery movement.
In both 2022 and 2023, about 1 in 4 people who needed treatment got it—so no major progress yet.
What’s the Big Picture
Between 2021 and 2023, most trends show stability, not sharp change. The big shifts—like the rise in cannabis use, vaping, and mental health issues—largely happened earlier, between 2015 and 2021.
Now, we seem to be in a holding pattern:
- Higher cannabis use is here to stay—but not necessarily rising fast anymore.
- Mental health concerns remain elevated, but may be plateauing.
- Cigarette smoking continues to fall, while vaping grows.
- Teen alcohol use is slowly declining.
- Addiction rates are high, but not growing.
- Access to treatment remains a major gap.
- Recovery is gaining ground.
It’s a mixed bag. Some trends are improving. Some aren’t getting worse. And some, like vaping, are still heading in the wrong direction. What happens in the next couple of years will be key to understanding our progress. It will show whether we’ve truly turned a corner or are simply catching our breath before the next wave.
Why This Matters
Let’s be honest: when you’re scrolling through stats about addiction or mental health, it can feel overwhelming. All those numbers and percentages—what do they really mean for real people, real families, real communities?
Here’s the bottom line: these numbers matter because they reflect lives—millions of them. Let’s break it down.
1. These Are People, Not Just Stats
Every data point in this report represents someone’s story. That “48 million” living with a substance use disorder? That’s not just a number. That’s parents, siblings, neighbors—people you know. When we read that 3.2 million teens thought seriously about suicide last year, it’s not just a chilling statistic—it’s a wake-up call. These struggles aren’t happening in some distant place. They’re happening in our schools, our workplaces, and across kitchen tables. Almost half of young adults are struggling with mental health or addiction. That’s our next generation, trying to build futures while battling invisible wounds. And when those wounds go untreated, the ripple effects are enormous—lost lives, overloaded healthcare systems, broken families, and communities in crisis.
2. Prevention and Early Action Work
Most of these challenges don’t pop up overnight. They start early—during the teen years or in young adulthood. That’s why it matters that 1 in 7 teens is drinking, or that 11% are using marijuana. These early habits can pave the way to much bigger struggles down the road. And it’s not just about drugs—spotting the early signs of anxiety or depression can literally save a life.Here’s the thing: we have a chance to step in before things spiral. Parents, teachers, doctors—this is your window. If you know that vaping is now one of the top substances teens are using, treat that vape pen with the same concern you’d show a bottle of vodka. Prevention programs, school mental health support, honest conversations at home—these are tools that work if we use them. But we have to act early and consistently.
3. Data Can Guide Better Decisions if We Pay Attention
These numbers can, and should, guide where we put our time, energy, and money. For example, if most opioid misuse stems from prescription medications, that signals a clear need. We must continue tightening prescribing guidelines and expanding access to treatment. Alcohol is still the most widely used (and misused) substance—so no, we can’t ignore that just because there’s a fentanyl crisis. When youth mental health worsens across the board, the message is clear. We need more school counselors, stronger youth services, and visible, accessible suicide prevention efforts that are taken seriously.
Let’s also not forget the massive treatment gap. 75% of people with substance use disorders don’t get help. That’s not a failure of willpower; it’s a failure of access. We need policies that make getting help easier, not harder. More treatment centers. Better insurance coverage. Services in rural areas. Telehealth options. The data points to the gaps, we just have to close them.
4. We Need to Talk About This Openly
Stigma is still one of the biggest barriers to people getting help. Many don’t reach out because they’re ashamed or afraid of being judged. But when 1 in 5 adults has a mental health condition, it’s time to call it what it is: common. And treat it like we would any other health issue. No shame, just support.
The more we talk about these issues—at home, in schools, on social media—the more we normalize getting help. That awkward conversation about your teen vaping? It could change their trajectory. That town meeting about overdose deaths? It could spark a lifesaving initiative. And every time we speak openly, we chip away at the stigma and create space for recovery.
5. It’s Not One Fix, It’s All of Them
Substance use and mental health issues aren’t simple problems, so there’s no one-size-fits-all solution. It’s not just about rehab, or laws, or education—it’s all of the above. Want to reduce addiction long term? Start by addressing youth mental health. Want to lower overdose deaths? Distribute naloxone. Want to stop the cycle of incarceration? Fund treatment alternatives for nonviolent offenders. We need to tackle this from every angle:
- Mental health and substance use support in schools
- Easier access to quality treatment
- Support systems for people in recovery (jobs, housing, community)
- Targeted harm-reduction efforts (like fentanyl test strips, overdose reversal meds)
- Ongoing research to keep up with new drug trends
The report is basically a roadmap—it tells us where the pain points are, and what we can do about them. But action is up to us.
6. There’s Still Hope, But We Must Act Now
Yes, these numbers are urgent. Some are terrifying. The overdose crisis is a public health emergency. But there’s also hope in the data. Millions of people are recovering. Some risky trends are leveling off. And history shows us we can make progress. Look at smoking, HIV, teen pregnancy—huge shifts happened because we prioritized them.
We can do the same here, but it’s going to take sustained, national-level commitment. This isn’t a side issue. When nearly 60% of Americans are using substances and almost a quarter are experiencing mental health challenges, this is the health crisis of our time.
The Bottom Line
These numbers aren’t just statistics. They’re stories. They’re signals. And they’re a call to action. They show us where to focus our compassion, our policies, and our resources.
If you’ve ever wondered what you can do—start here. Share the data. Talk about the issues. Support prevention. Advocate for access to care. Help someone you love take that first step toward recovery.
The numbers tell us what’s happening. It’s up to all of us to change what happens next.
Sources: This report is based on data from the Substance Abuse and Mental Health Services Administration’s (SAMHSA) 2023 National Survey on Drug Use and Health and related publications, including the 2023 NSDUH Annual National Report, the Highlights from the 2023 NSDUH, and comparison data from 2021 and 2022 NSDUH reports. Additional context and statistics were drawn from the NSDUH Veterans analysis and other research (Recent Trends in Mental Health and Substance Use Concerns Among Adolescents | KFF) to provide historical perspective. All numeric references correspond to the NSDUH findings as cited throughout this document.
Start Your Journey
Contact us today and one of our team member will get in touch with you shortly.
INFORMATION REQUEST
CONTACT INFORMATION
ADDRESS
23712 Birtcher Drive ,
Lake Forest, CA 92630
PHONE:
866-955-1607
EMAIL:
ADMISSIONS@12SOUTHRECOVERY.COM